700 Glenhuntly Road
Caulfield VIC 3162
03 9044 4555

700 Glenhuntly Road
Caulfield VIC 3162
03 9044 4555
Knee Osteoarthritis
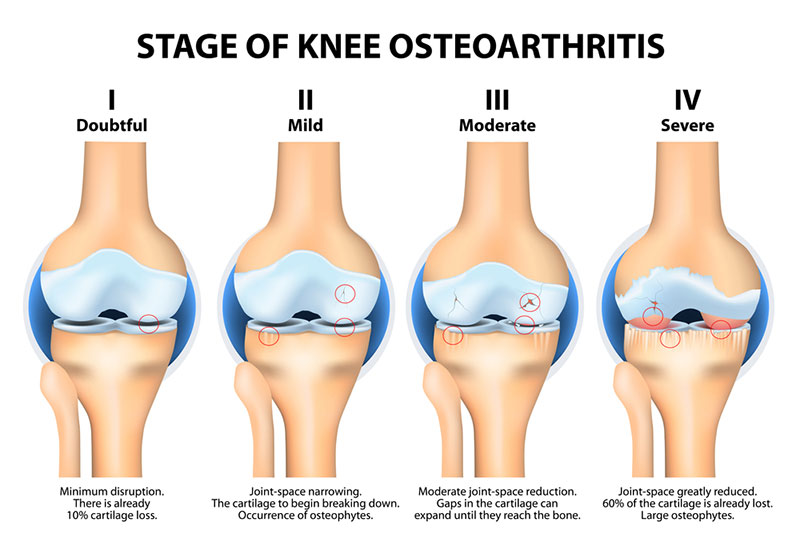
Osteoarthritis of the knee is a very common orthopaedic condition and can have significant impact on the quality of life of individual patients and the community as a whole.
A thick layer of protective cartilage covers the bones of the normal knee joint. This cartilage has many functions including providing the knee with a very low friction surface to allow for ease of motion. When this cartilage wears away, exposed bony surfaces develop which is essentially the process of osteoarthritis.
The causes for the development of osteoarthritis are not fully understood, however there are many factors thought to be involved. Sometimes there is a hereditary predisposition, i.e. it runs in families. Females tend to be affected more than males and there is a strong link with obesity. Injuries to the knee may have a significant role to play, especially where there has been previous cruciate ligament, meniscus and cartilage injuries.
A thick layer of protective cartilage covers the bones of the normal knee joint. This cartilage has many functions including providing the knee with a very low friction surface to allow for ease of motion. When this cartilage wears away, exposed bony surfaces develop which is essentially the process of osteoarthritis.
The causes for the development of osteoarthritis are not fully understood, however there are many factors thought to be involved. Sometimes there is a hereditary predisposition, i.e. it runs in families. Females tend to be affected more than males and there is a strong link with obesity. Injuries to the knee may have a significant role to play, especially where there has been previous cruciate ligament, meniscus and cartilage injuries.
When end-stage arthritis occurs, there may be significant pain during weight-bearing activity such as walking, kneeling or squatting. In some instances certain regions of the knee are painful after holding the knee in a prolonged position (e.g. after sitting through a feature length movie). This pain is accentuated as the knee is loaded down with body weight, heavy force or strenuous muscle activity. Eventually the pain may go on to become present at night time, and this may be due to the release of inflammatory chemicals into the knee joint due to the breakdown of tissue. Other symptoms may include stiffness, swelling, limping or a sensation of grating or crunching from within the knee.
Treatment of osteoarthritis may be surgical or non surgical. Generally, non-surgical treatment should be exhausted prior to surgical management.
Physiotherapy and exercises:
This aims to strengthen the muscles around the knee and optimise the range of motion of the knee. This may be achieved initially by using an exercise bike, which also is a low impact way of burning calories and losing weight. Weight loss may also be achieved with a balanced diet, and expert dietary opinion may be needed in some cases. Muscle strengthening, improved range of motion and weight loss will aid walking ability and further endurance and weight loss.
Pain killers:
Initially simple painkillers such as regular paracetamol should be used. This is usually taken 1 gram (2x 500mg tablets) every 6 hours. You should not exceed 8x 500mg tablets in one day.
Anti inflammatory medication usually works synergistically with paracetamol to improve its effects. There are many types of this medication (e.g. Mobic, Voltaren, Naprosyn or Celebrex), however they may lead to certain side effects such as stomach upset and potentially stomach ulceration, aggravation of high blood pressure or heart conditions as well as worsening of any pre-existing kidney problems. Use of these medications, and other stronger painkillers should be discussed with your surgeon or general practitioner.
Mobility aids:
These include walking sticks, four point frames and others. The aim of these devises is to offload pressure on the knee joint. Usually a walking stick works best if is held in the opposite hand to the affected knee i.e. if the right knee is affected, then the stick is held the left had and vice versa.
Injections:
Injections into the knee joint may be of two different types:
This preparation reduces pain within the knee by targeting nerve endings with the local anaesthetic and also by reducing inflammation in the knee with the corticosteroid. This effect may last up to 3 months and recurrence of symptoms is common thereafter. Repeat injection is possible, however if performed frequently, increases the risk of infection into the knee joint.
Viscosupplementation
This preparation is made up of a substance known as hyaluronic acid, one of the components of the natural cartilage of all joint surfaces. There is some evidence to suggest that this injection may aid pain relief for between 3 to six months. Like other forms of non-operative treatment, it does not cure arthritis, rather aims to reduce pain.
Once non-surgical treatment has been tried and exhausted, surgical management of osteoarthritis may be performed. There are three main options for surgical management:
Arthroscopy
This is also known as keyhole surgery and is usually very safe and well tolerated procedure. The aim of surgery where there is arthritis is to “clean up” any loose or unstable flaps of cartilage and meniscus, which may be present in conjunction with the arthritic process. Where symptoms are thought to be related to these pathologies, rather than due to the pain related to arthritis, outcomes are usually satisfactory. It is possible, however for any underlying arthritic symptoms to be exaggerated after this procedure. Arthroscopy does not cure the joint from arthritis or slow its progression.
Osteotomy
Osteotomy of the lower limb is a form of realignment surgery, which aims to offload part of the joint affected by arthritis. This surgery is successful in certain circumstances where there is limb deformity, early arthritis and results are best in those under 55 years of age. This procedure does not cure the arthritis, however is a good source of pain relief and put off the need for joint replacement whilst continuing to be active.
Replacement surgery
Knee joint replacement surgery involves the removal of the arthritic parts of the knee and replacement with an artificial joint. Either the whole of the knee joint may be replaced with a total knee joint or in certain cases only part of the knee joint which is affected may be replaced with a partial or unicompartmental knee replacement. The indications for which type of replacement is best discussed with your surgeon on an individual basis.
In general, knee joint replacement is usually delayed for as long as possible due to concerns with wear and loosening and the potential need for revision surgery in a young patient in the future. Revision surgery is much more complex with generally poorer results. In addition, total knee replacement is only suitable for activities such as golf, social doubles tennis and cycling. It is not compatible with certain high impact sports such as running and jumping, where early loosening of the components may occur.
Treatment of osteoarthritis may be surgical or non surgical. Generally, non-surgical treatment should be exhausted prior to surgical management.
Non-Surgical Treatment
Physiotherapy and exercises:
This aims to strengthen the muscles around the knee and optimise the range of motion of the knee. This may be achieved initially by using an exercise bike, which also is a low impact way of burning calories and losing weight. Weight loss may also be achieved with a balanced diet, and expert dietary opinion may be needed in some cases. Muscle strengthening, improved range of motion and weight loss will aid walking ability and further endurance and weight loss.
Pain killers:
Initially simple painkillers such as regular paracetamol should be used. This is usually taken 1 gram (2x 500mg tablets) every 6 hours. You should not exceed 8x 500mg tablets in one day.
Anti inflammatory medication usually works synergistically with paracetamol to improve its effects. There are many types of this medication (e.g. Mobic, Voltaren, Naprosyn or Celebrex), however they may lead to certain side effects such as stomach upset and potentially stomach ulceration, aggravation of high blood pressure or heart conditions as well as worsening of any pre-existing kidney problems. Use of these medications, and other stronger painkillers should be discussed with your surgeon or general practitioner.
Mobility aids:
These include walking sticks, four point frames and others. The aim of these devises is to offload pressure on the knee joint. Usually a walking stick works best if is held in the opposite hand to the affected knee i.e. if the right knee is affected, then the stick is held the left had and vice versa.
Injections:
Injections into the knee joint may be of two different types:
- Corticosteroid and local anaesthetic
This preparation reduces pain within the knee by targeting nerve endings with the local anaesthetic and also by reducing inflammation in the knee with the corticosteroid. This effect may last up to 3 months and recurrence of symptoms is common thereafter. Repeat injection is possible, however if performed frequently, increases the risk of infection into the knee joint.
This preparation is made up of a substance known as hyaluronic acid, one of the components of the natural cartilage of all joint surfaces. There is some evidence to suggest that this injection may aid pain relief for between 3 to six months. Like other forms of non-operative treatment, it does not cure arthritis, rather aims to reduce pain.
Surgical Treatment
Once non-surgical treatment has been tried and exhausted, surgical management of osteoarthritis may be performed. There are three main options for surgical management:
Arthroscopy
This is also known as keyhole surgery and is usually very safe and well tolerated procedure. The aim of surgery where there is arthritis is to “clean up” any loose or unstable flaps of cartilage and meniscus, which may be present in conjunction with the arthritic process. Where symptoms are thought to be related to these pathologies, rather than due to the pain related to arthritis, outcomes are usually satisfactory. It is possible, however for any underlying arthritic symptoms to be exaggerated after this procedure. Arthroscopy does not cure the joint from arthritis or slow its progression.
Osteotomy
Osteotomy of the lower limb is a form of realignment surgery, which aims to offload part of the joint affected by arthritis. This surgery is successful in certain circumstances where there is limb deformity, early arthritis and results are best in those under 55 years of age. This procedure does not cure the arthritis, however is a good source of pain relief and put off the need for joint replacement whilst continuing to be active.
Replacement surgery
Knee joint replacement surgery involves the removal of the arthritic parts of the knee and replacement with an artificial joint. Either the whole of the knee joint may be replaced with a total knee joint or in certain cases only part of the knee joint which is affected may be replaced with a partial or unicompartmental knee replacement. The indications for which type of replacement is best discussed with your surgeon on an individual basis.
In general, knee joint replacement is usually delayed for as long as possible due to concerns with wear and loosening and the potential need for revision surgery in a young patient in the future. Revision surgery is much more complex with generally poorer results. In addition, total knee replacement is only suitable for activities such as golf, social doubles tennis and cycling. It is not compatible with certain high impact sports such as running and jumping, where early loosening of the components may occur.
The information above is general. All surgical procedures involve some risk. If you would like advice on your specific condition, please contact Oasis Orthopaedics to make an appointment with one of our specialists.