700 Glenhuntly Road
Caulfield VIC 3162
03 9044 4555

700 Glenhuntly Road
Caulfield VIC 3162
03 9044 4555
Knee Replacement
Knee replacement is a surgical treatment option for arthritis of the knee. It involves the removal of the arthritic surfaces of the knee joint and replacement with an artificial joint surface. The artificial joint is usually made out of a combination of low friction metals separated by a high-density polyethylene. Long-term pain relief is provided by removing the arthritic component of the joint where pain may have been otherwise generated by bone moving on bone during walking. Knee replacement may be a total or partial knee replacement depending on whether all of the joint or only part of the joint has been affected by arthritis.
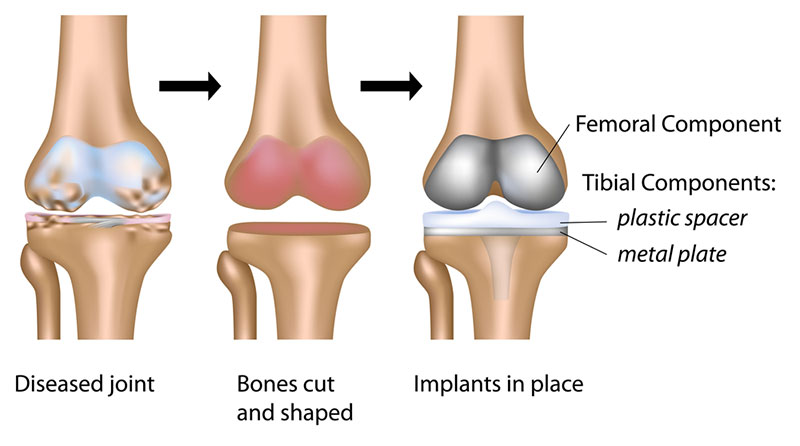
Total Knee Replacement is a procedure performed when more than once compartment of the knee is affected by arthritis. The arthritic surfaces of the distal femur and proximal tibia (and sometimes the patella) are removed and replaced with a metallic surface which bonds to the distal femur and a metallic tray that bonds to the proximal tibia. The tibial tray has a high density, polyethylene liner that firmly clips in to the tray to lock it in place. This metal configuration allows flexion and extension of the knee, and a smaller amount of translation and rotation, similar in nature to the mechanics of the natural knee.
In removing the arthritic surfaces, the painful stimuli are removed, restoring range of movement. During the procedure the anterior cruciate ligament is routinely removed, but the posterior cruciate may be removed or retained, depending on the design of the knee replacement. The collateral ligaments are preserved, but frequently they need to be loosened from their attachment to the tibia to help straighten the knee joint and permit more movement of the knee.
During the procedure, local anaesthetic is usually infiltrated into the tissues of the knee to reduce post-operative pain. This is a very important component to the surgery as pain reduction post operatively is crucial to permit early mobilisation and range of motion. Rehabilitation following a total knee replacement is critical to the long-term outcome of the procedure.
The procedure may be performed either under a general anaesthetic or spinal anaesthetic. These options may be discussed with the anaesthetist. The average hospital stay is usually around 4 nights.
Total Knee Replacement
Total Knee Replacement is a procedure performed when more than once compartment of the knee is affected by arthritis. The arthritic surfaces of the distal femur and proximal tibia (and sometimes the patella) are removed and replaced with a metallic surface which bonds to the distal femur and a metallic tray that bonds to the proximal tibia. The tibial tray has a high density, polyethylene liner that firmly clips in to the tray to lock it in place. This metal configuration allows flexion and extension of the knee, and a smaller amount of translation and rotation, similar in nature to the mechanics of the natural knee.
In removing the arthritic surfaces, the painful stimuli are removed, restoring range of movement. During the procedure the anterior cruciate ligament is routinely removed, but the posterior cruciate may be removed or retained, depending on the design of the knee replacement. The collateral ligaments are preserved, but frequently they need to be loosened from their attachment to the tibia to help straighten the knee joint and permit more movement of the knee.
During the procedure, local anaesthetic is usually infiltrated into the tissues of the knee to reduce post-operative pain. This is a very important component to the surgery as pain reduction post operatively is crucial to permit early mobilisation and range of motion. Rehabilitation following a total knee replacement is critical to the long-term outcome of the procedure.
The procedure may be performed either under a general anaesthetic or spinal anaesthetic. These options may be discussed with the anaesthetist. The average hospital stay is usually around 4 nights.
Partial Knee Replacement
In some instances, a knee joint may develop arthritis in only one compartment i.e. only the medial, lateral or patella-femoral compartments. The other compartments tend to be well preserved. If there is such localised arthritis, it may be possible in some patients to replace only that portion of the knee that is damaged, leaving the normal remaining two compartments untouched. This is known as a unicompartmental or partial knee replacement. Most commonly this is done for the medial compartment, although the patello-femoral and lateral compartments can also be replaced independently.
Partial knee replacements can provide an excellent range of pain-free movement and very rapid recovery as the operation is usually done through a smaller incision than a conventional total knee replacement and less tissue is disturbed. The design philosophy is that there is less bone removed during a partial replacement, leaving more of the native bone and ligaments intact. A major difference between total and partial knee replacement is the preservation of the anterior cruciate ligament (ACL) in a partial knee replacement. The ACL is a very important knee stabilizer and also aids with proprioception (the sense of knowing where your limb is in space). A partial knee replacement may be converted to a total knee replacement, usually in the setting of progression of arthritis to other compartments within the knee.
The drawbacks of this procedure is that it is not suitable for all patients, specifically if there are symptoms from more than one region in the knee, if there is significant deformity or stiffness, or if there is a generalised inflammatory cause of arthritis such as rheumatoid arthritis.
When is the Right Time to Have My Knee Replaced?
In general, when you find that your symptoms are intrusive in your day-to-day life, despite having tried all the non-operative treatments, then this is usually a good guide as to when you may want to consider Knee Replacement. This may include uncontrollable pain despite using analgesics and anti-inflammatories, significant disturbance of sleep, reduced walking distance or endurance, or if there is a progressive deformity or substantial stiffness of the knee such that day-to-day activities such as managing stairs, putting on shoes, socks or pantyhose is a major effort.
Why Shouldn’t I Have My Knee Replacement Straight Away?
While total knee replacement is an excellent operation with regards to pain relief in over 80% of patients, large studies have shown that up to 20% of patients may still be “dissatisfied” with the results of their knee replacement. The reasons for this are not clear, despite having had an technically well done operation, although it may have a lot to do with the multiple complex movements that a knee replacement is required to cope with and the new stresses applied to the tissues surrounding the replaced knee.
When a knee replacement fails to function satisfactorily, then it may require a revision knee replacement. Each time a knee is revised there is loss of bone and the results become somewhat less predictable and possibly less durable than the initial total knee replacement. Moreover, the younger or more active the patient is at the time of their total knee replacement, the shorter the anticipated lifespan of the prosthesis, due to the amount of cycles the knee may be required to do.
Potential Complications
No surgery is without the potential for complications. These can be classified as general complications and those specific to this operation.
General complications
These complications relate to all types of orthopaedic surgery and include those related to the anaesthetic, wound site infection, bleeding and damage to nerves and blood vessels. Lower limb orthopaedic surgery also carries the risk of deep venous thrombosis and pulmonary embolism (DVT and PE). Please refer to the General Orthopaedic Surgical Complications information sheet for further details of these complications.
Specific Complications for Knee Replacement
Infection
Infection carries a bigger potential risk in relation to joint replacement. This is due to the components being artifical, and difficulty in fully eliminating the infection. If infection occurs, treatment often involves readmission to hospital, administration of intravenous antibiotics and potentially further surgery. Where surgical removal of the infection fails, it may be necessary to remove the knee replacement and replace it with an antiobitic loaded knee joint spacer while the infection clears. In rare instances the knee joint may need to be permanently stiffened (arthrodesis).
Wear and Loosening
Over time, the polyethylene component of the knee replacement may wear. Tiny particles are created during the wearing process, which the body reacts to. This reaction can lead to pain and possibly loosening of the fixed components on the femur, tibia and patella. If there is loosening, it may be necessary to revise or redo the knee replacement. Revision surgery is usually much more complicated that the primary operation and results tend to be less satisfactory overall.
Stiffness and swelling
Stiffness and swelling is common after a knee replacement. Sometimes stiffness persists and affects regaining satisfactory range of motion. Early pain relief and physiotherapy tends to reduce this, however when stiffness continues to be a problem it may be necessary to manipulate the knee under an anaesthetic to regain range of motion. This may involve 2 to 4 nights admission in hospital.
The information above is general. All surgical procedures involve some risk. If you would like advice on your specific condition, please contact Oasis Orthopaedics to make an appointment with one of our specialists.