700 Glenhuntly Road
Caulfield VIC 3162
03 9044 4555

700 Glenhuntly Road
Caulfield VIC 3162
03 9044 4555
Patellofemoral Instability
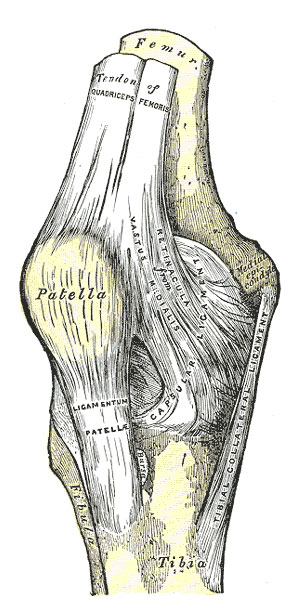
Fig 345. Henry Gray - Anatomy of the Human Body. 1918.
Patellofemoral instability refers to a spectrum of symptoms relating to the instability of the kneecap joint. There are a large variety of symptoms that are experienced with this condition and include the feeling of the knee cap wanting to move too far laterally, but not completely out of joint (subluxation), all the way to having a complete kneecap dislocation. When complete kneecap dislocation occurs more than once in the same knee is it referred to as Episodic Patella Dislocation (EPD). After one patella dislocation, the chance of EPD occurring can be as high as 40% to 70%.
EPD can cause significant short and long-term problems to the knee. In the short term, recurrent dislocations cause pain and prolonged rehabilitation once the patella is reduced. The dislocation itself often leads to rupture of the Medial Patello Femoral Ligament (MPFL) and may be associated with damage to the knee cartilage in up to 90% of cases. The MPFL acts as a restraint to patella dislocations, so if it is torn during the first dislocation, it is often a factor contributing to EPD. In the long term if EPD is left untreated, it is often associated with the progression of arthritis within the patellofemoral compartment of the knee.
There are multiple contributing factors to EPD. The shape of the patellofemoral joint and especially how the patella and femur match up with each other is the issue in most patients.
The most common anatomy problem observed is related to the groove on the end of the femur, where the patella is supposed to run. When this groove (called the trochlea) is misshapen it is called trochlea dysplasia (TD). TD has varying degrees of severity, ranging from flattening of the groove all the way to having a bump (or convex surface) rather than a groove. TD is mild in most patients with EPD, however it occurs in up to 96% of patients with EPD compared to 3% of patients without EPD.
Other common causes of EPD include where the patella sits too high above the trochlea (patella alta) and malalignment of the lower limb. Often there is more than one anatomical cause, and there is usually associated poor function of an injured MPFL.
The diagnosis as to which factors are involved in EPD are incredible variable, and are assessed by physical examination and medical imaging. The latter usually involved plain x-rays and an MRI. Based on the analysis of your physical examination and medical imaging the surgeon will then be able to discuss the options available to you for treatment.
Non-surgical treatment is usually prescribed when there has been only one or two patella dislocations without an anatomical cause or there is untreated feelings of subluxation. Physiotherapy is very useful in this scenario to strengthen the weakened quadriceps muscles, in particular vastus medialis obliquus (VMO). Other treatment instituted may include stretching exercises for the lateral soft tissues around the knee as well as patella taping and bracing.
When non-operative treatment has failed and/or where there is an anatomical cause for EPD, then it may be suitable to undergo surgical management.
The surgical prescription aims at addressing one or all of the abnormal anatomy that leads to the dislocation. French orthopaedic surgeons, who have been considered the pioneers of patellofemoral stabilization surgery coined this the “à la carte” treatment philosophy.
Where TD is significant and considered to be the main contributing factor, then a procedure to reshape the trochlea groove to match the patella may be performed. This procedure is called a trochleoplasty, and is less commonly performed than other procedures.
When patella alta is seen to be the main factor, then a procedure may be performed to bring the patella down to an appropriate height such that it fits the trochlea. This is called a tibial tubercle osteotomy and involves cutting the bone at the front of the tibia where the patella tendon attaches and reattaching the bone with the tendon still attached further down the tibia. Two screws are usually used to fix the bone back down. This is often combined with a small soft-tissue realignment of the tissues surrounding the patella to fine tune the movement of the patella. Tibial tubercle osteotomy may be performed alone or in combination with other stabilizing procedures.
Frequently, the MPFL is ruptured and/or poorly functioning, in which case reconstruction of the MPFL ligament can be performed. This procedure often involves using one of the hamstring tendons that is then attached to the patella and tunneled underneath the soft tissue on the inner side of the knee to be attached to the corresponding location on the femur. The aim of this is to restore the MPFL function and prevent further dislocation. MPFL reconstruction may be performed alone or in combination with other stabilising procedures.
In most of these stabilisation procedures, an arthroscopy (key hole surgery) is performed at the same time to assess/treat any cartilage damage and to confirm and ensure that a satisfactory result of the stabilisation procedure has occurred.
Recovery from these procedures is on an individual basis depending on which procedure, or combination of procedures, have been performed. Usually, the hospital stay is from two to three nights, and there may be the need for a knee brace and crutches to be used for 6 to 8 weeks, especially following tibial tubercle osteotomy. Postoperative x-rays are usually needed after procedure.
EPD can cause significant short and long-term problems to the knee. In the short term, recurrent dislocations cause pain and prolonged rehabilitation once the patella is reduced. The dislocation itself often leads to rupture of the Medial Patello Femoral Ligament (MPFL) and may be associated with damage to the knee cartilage in up to 90% of cases. The MPFL acts as a restraint to patella dislocations, so if it is torn during the first dislocation, it is often a factor contributing to EPD. In the long term if EPD is left untreated, it is often associated with the progression of arthritis within the patellofemoral compartment of the knee.
There are multiple contributing factors to EPD. The shape of the patellofemoral joint and especially how the patella and femur match up with each other is the issue in most patients.
The most common anatomy problem observed is related to the groove on the end of the femur, where the patella is supposed to run. When this groove (called the trochlea) is misshapen it is called trochlea dysplasia (TD). TD has varying degrees of severity, ranging from flattening of the groove all the way to having a bump (or convex surface) rather than a groove. TD is mild in most patients with EPD, however it occurs in up to 96% of patients with EPD compared to 3% of patients without EPD.
Other common causes of EPD include where the patella sits too high above the trochlea (patella alta) and malalignment of the lower limb. Often there is more than one anatomical cause, and there is usually associated poor function of an injured MPFL.
The diagnosis as to which factors are involved in EPD are incredible variable, and are assessed by physical examination and medical imaging. The latter usually involved plain x-rays and an MRI. Based on the analysis of your physical examination and medical imaging the surgeon will then be able to discuss the options available to you for treatment.
Non-Operative Treatment
Non-surgical treatment is usually prescribed when there has been only one or two patella dislocations without an anatomical cause or there is untreated feelings of subluxation. Physiotherapy is very useful in this scenario to strengthen the weakened quadriceps muscles, in particular vastus medialis obliquus (VMO). Other treatment instituted may include stretching exercises for the lateral soft tissues around the knee as well as patella taping and bracing.
Operative Treatment
When non-operative treatment has failed and/or where there is an anatomical cause for EPD, then it may be suitable to undergo surgical management.
The surgical prescription aims at addressing one or all of the abnormal anatomy that leads to the dislocation. French orthopaedic surgeons, who have been considered the pioneers of patellofemoral stabilization surgery coined this the “à la carte” treatment philosophy.
Where TD is significant and considered to be the main contributing factor, then a procedure to reshape the trochlea groove to match the patella may be performed. This procedure is called a trochleoplasty, and is less commonly performed than other procedures.
When patella alta is seen to be the main factor, then a procedure may be performed to bring the patella down to an appropriate height such that it fits the trochlea. This is called a tibial tubercle osteotomy and involves cutting the bone at the front of the tibia where the patella tendon attaches and reattaching the bone with the tendon still attached further down the tibia. Two screws are usually used to fix the bone back down. This is often combined with a small soft-tissue realignment of the tissues surrounding the patella to fine tune the movement of the patella. Tibial tubercle osteotomy may be performed alone or in combination with other stabilizing procedures.
Frequently, the MPFL is ruptured and/or poorly functioning, in which case reconstruction of the MPFL ligament can be performed. This procedure often involves using one of the hamstring tendons that is then attached to the patella and tunneled underneath the soft tissue on the inner side of the knee to be attached to the corresponding location on the femur. The aim of this is to restore the MPFL function and prevent further dislocation. MPFL reconstruction may be performed alone or in combination with other stabilising procedures.
In most of these stabilisation procedures, an arthroscopy (key hole surgery) is performed at the same time to assess/treat any cartilage damage and to confirm and ensure that a satisfactory result of the stabilisation procedure has occurred.
Recovery from these procedures is on an individual basis depending on which procedure, or combination of procedures, have been performed. Usually, the hospital stay is from two to three nights, and there may be the need for a knee brace and crutches to be used for 6 to 8 weeks, especially following tibial tubercle osteotomy. Postoperative x-rays are usually needed after procedure.
Potential Complications
No surgery is without the potential for complications. These can be classified as general complications and those specific to this operation.
General complications
These complications relate to all types of orthopaedic surgery and include those related to the anaesthetic, wound site infection, bleeding and damage to nerves and blood vessels. Lower limb orthopaedic surgery also carries the risk of deep venous thrombosis and pulmonary embolism (DVT and PE). Please refer to the General Orthopaedic Surgical Complications information sheet for further details of these complications. Regarding patellofemoral stabilisation surgery in particular, there is the potential for ongoing instability and pain to persist.
Specific Complications for Patello-femoral Stabilisation Procedures
Trochleoplasty
- Delayed and Non-Union
This may occur on the undersurface of the trochlea cartilage, however it is a very uncommon complication. Further surgery may be required to address this. - Necrosis of the cartilage layer
This refers to the overlying trochlea cartilage not having enough blood supply and gradually dying. This is a very uncommon complication, however the repercussions are significant and may lead to the need for further surgery in the form of patellofemoral replacement.
Tibial Tubercle Osteotomy
- Delayed Union and Non Union
This refers to slow (or no) bone healing at the tibial tubercle osteotomy site. This may occur because the bone has been cut and needs time to heal. Delayed healing may be due to a number of causes and all of these are addressed should this issue arise. More surgery may be required to encourage to bone to heal faster in some settings. - Fracture
Once again, as the bone is being cut, there is the potential for fracture to occur into the joint or below the joint level. This is usually dealt with at the time of surgery if it occurs. - Ongoing Pain
If pain persists following an osteotomy this may be due to many different causes, which is best assessed by the treating surgeon. Potential reasons include non-union and pain related to prominent metal ware used to stabilize the osteotomy. The metal may be removed at a later date once the osteotomy has healed and full function has been regained. This is an individual decision and different surgeons have different opinions regarding metal ware removal and the timing for this. This is best discussed with the surgeon individually.
MPFL Reconstruction
- Patella Fracture
This is an uncommon complication, however may occur at the site where the MPFL graft is attached to the patella. If this does occur, it may lead to being in a brace until the fracture heals or even potentially needing further surgery to fix the fracture. - Medial sided knee pain
There is often early pain on the inner side of the knee following this procedure, which, usually stems from the graft attachment to the patella. The other source of pain may be related to the graft site for the hamstring tendon. Both usually settle down by themselves over time. Pain related to metal ware fixation in the femur is uncommon, however should it be a long-term issue, removing the metal ware may be discussed with the treating surgeon. Fixation is usually not removed until the graft has fully attached to the femur and a full rehabilitation has been achieved.
The information above is general. All surgical procedures involve some risk. If you would like advice on your specific condition, please contact Oasis Orthopaedics to make an appointment with one of our specialists.